Solutions
Customer Support
Resources
Payer contract management is important in handling the relationship between payer organizations and healthcare providers.
Read on to discover what it is, and how contract management software can help.
But before we dive into the benefits of payer contract management software and how to choose the right solution, who is a payer, and what is payer contract management?
A ‘payer’ refers to an entity or business that pays for services rendered by a healthcare provider. This payer could refer to a commercial insurance company, government program, employer, or patient.
Payers are usually used by practicing physicians, who may come into contact with a variety of clauses when negotiating the terms and conditions of payment for services. Physicians might also contract with third-party administrators or intermediary contracting entities, including other healthcare providers who have assumed financial risk from a payer.
Healthcare organizations and payer organizations all require agreements to be made over the terms and conditions for medical services, coverage, and payment. In fact, managing payer contracts is one of the primary challenges of healthcare providers.
Payer contract management is the process of managing these contracts and tracking the difference between revenue generation for each individual payer. Without effective payer contract management, healthcare providers are limited in their ability to see if they are being paid correctly.
The goal of payer contract management is to standardize contracts and make them as consistent as possible, while maintaining beneficial terms.
Most standard contract management best practices apply to payer contracts. However, there are a few notable differences between payer contracts and other types of business contracts.
Payer contracts often involve detailed reimbursement models, such as fee-for-service, capitation, or value-based care agreements. Managing these requires tools and expertise to account for payment schedules, performance metrics, and shared-risk arrangements. In contrast, standard business contracts may focus more on fixed terms, pricing, and deliverables.
Payer contracts must adhere to strict healthcare regulations, such as the Affordable Care Act (ACA) or the Stark Law, and often include obligations related to patient privacy under laws like HIPAA. Other contract types may not face the same level of legal scrutiny or regulatory oversight.
Payer contracts are frequently renegotiated due to changes in healthcare policies, reimbursement rates, or the scope of services offered. Unlike static commercial agreements, these contracts often evolve during their lifecycle to accommodate new terms or address disputes over claims and payments.
This means that those working with payer contracts, usually as part of a healthcare provider contract management process, have a few extra things to consider when handling these complex contracts. Let’s explore those in more detail now.
If you’re starting from scratch, it’s important to determine the current mix of payers your organization has and which ones are the most important to your organization. Analyzing your payer mix enables you to determine which of these payers you should prioritize in contracting efforts.
Consider your past relationship with them, the terms of their existing contract, and their overall track record. This can derisk your contracts further down the line, as you know what to expect from the partnership and may reduce the chance of disruptions and contractual disputes.
Payer contracts are value-based contracts, which means they often come with confusing terms, so it’s best to be clear about those terms from the get-go.
For example, payer contracts may extend remuneration based on factors such as bonus payments, bundled payments, or a more risk-based attribution. While others could rely on withholds, meaning that a set portion of expected payments are held and only released when certain conditions are met.
All these moving parts mean that it’s fairly easy for a payment to go wrong, no payer is going to tell you you mistakenly underpaid them! Consistency is key here, so using standardized or automated contract templates for your payer contract management will ensure you’re able to track and keep on top of terms.
The healthcare industry is hot on compliance, as the regulatory landscape is complex and ever-changing. As a result, healthcare providers and organizations have to deal with multiple stakeholders beyond just payers.
From regulatory requirements and privacy laws to provider-specific reimbursement structures and shifting payment models, payer contract management is complex. It’s important to monitor everything from delivery timelines to quality control and other contractual obligations.
If you don’t have a set source of truth for this information, it can be difficult to track and monitor your compliance. If you want to speed up this process, you’ll need a centralized contract repository and fully searchable contracts.
Want to know where to get started? Check out this simple guide to contract compliance.
{{quote1}}
As with monitoring compliance, it’s also incredibly important to take a proactive approach towards payer contract renewals. This allows you to negotiate more favorable terms, and revisit existing clauses and conditions before the contract terminates.
Payer contracts typically come with expiration dates meaning they can be renewed, renegotiated, or terminated. Auto-renew contracts can be problematic if payors are changing contract terms (especially rates) and changes are not transparent to a physician or healthcare organization.
A proactive approach involves setting up contract reminders over time to give you more time to make strategic decisions on how to approach a renewal.
Learn more about how to take charge of your contract renewals in this guide to renewal management.
Investing in contract management (CLM) software could be transformative for your payer contracts. A solution like Juro can allow healthcare organizations to create, agree, execute, and manage payer contracts up to 10x faster than traditional tools. Healthcare organizations using CLM can benefit from:
Juro’s AI-enabled contract automation platform empowers organizations to accelerate the creation, execution, and management of contracts. When it comes to payer contract management, software like Juro mitigates the risk of human error and missed renewals, helping you to be compliant.
You can find out more by hitting the banner below.

There are numerous CLMs out there to choose from, that’s why it’s important to consider the specifics of payer contracts and the challenges in managing them.
For example, when managed correctly payer contracts can lead to cost savings and improved quality of care as it facilitates the negotiation of reimbursement terms. This means you’ll benefit from strong contract negotiation features and contract tracking.
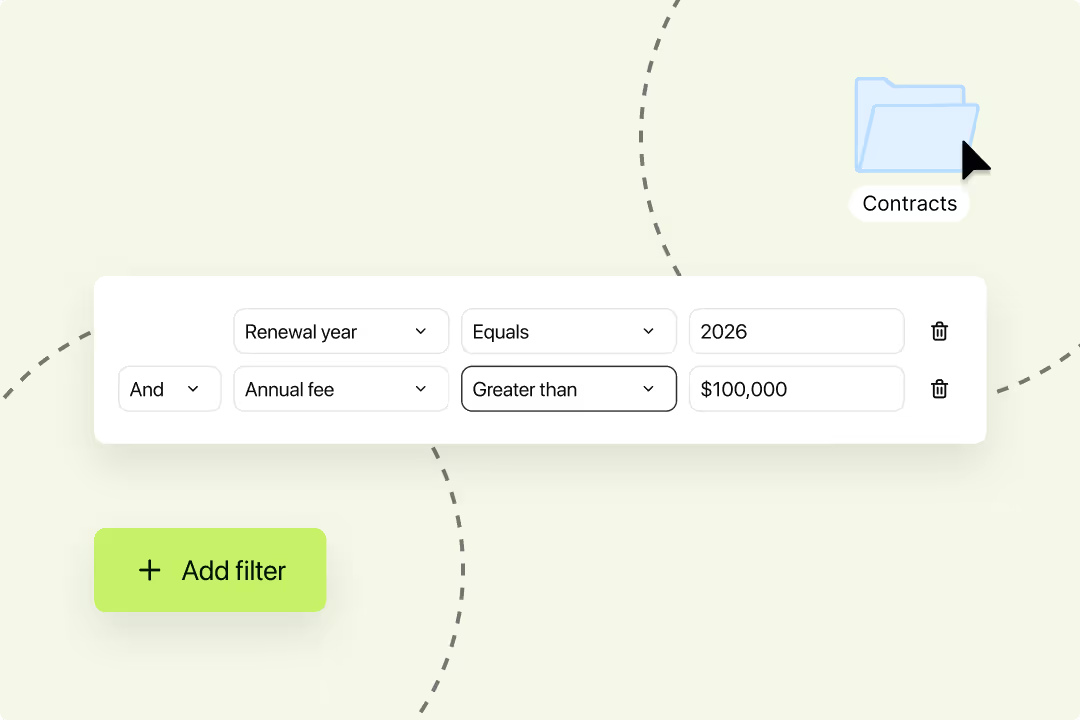
In order to track these contracts through every stage of the lifecycle, you'll need somewhere to store them and you want it to simplify how you search for specific agreements.
This alone is a dramatic improvement process where supplier contracts are stored as physical files, or scattered across shared drives. It also means you can quickly pull together those all-important files ahead of a fundraiser or due diligence process.
Juro makes this process even easier for healthcare organizations, with OCR search functionality that enables users to query contracts in seconds to find specific terms and values.
Juro's supplier contract management software also offers custom contract dashboards, making it easier than ever to filter and manage payer contracts at scale.
Juro's data-rich contract repository makes finding, tracking, and querying contracts quick and easy.
The complex regulatory landscape for healthcare-related contracts means that regulations change and you need to be able to keep on top of these when managing supplier contracts.
When it comes to payer contracts, key contract data can often be spread across several different places, and there's no single source of truth for things like renewal dates, or payment dates. This increases contract risk and could leave you in a dangerous situation when it comes to renegotiating favourable terms.
Fortunately, you can use contract management software like Juro to automate contract reminders for key deadlines. Users simply tag the dates as contract metadata and customize the frequency of the reminders based on their preferences.
The contract owner and relevant party will then be notified when the deadline is approaching, giving them instant visibility into important dates.
Complex contracts require negotiation, a contract management platform with AI functionality is a great way to save some time when reviewing and extracting data from contracts.
For example, Juro’s legal AI can be used to create and amend contracts, while setting guardrails for your drafting revising, and refining clauses. You can even use this AI functionality to identify legal risks in contracts or summarize contract terms in a format ready to share with stakeholders.

Juro is the trusted platform for 6000+ companies already streamlining their contract management and is a Leader in the CLM category according to G2. This makes it an obvious choice if you’re in the market for payer contract management software.
Juro’s end-to-end contract management platform includes automated templates, rich-text editor, and AI draft functionality, all working seamlessly with the features we listed above, enabling healthcare organizations like yours to streamline payer contract management.
If you’re interested in streamlining your contract management process today, book a demo with the form below.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.

